The cornea is a very important structure on the front part of the eye which is one of the structures responsible for focusing light onto the retina. Keratoconus is a non-inflammatory eye condition that affects this structure by causing the central cornea to thin and sag, causing a decrease in vision.

image source from American Academy of Ophthalmology
Currently there is no known cause of keratoconus, however genetics does play a part in the presentation of this disease. Therefore, having a family member with this condition can increase the risk of getting this disease as well. According to the Raine Study 1 in 84 Australian Adults in their 20’s have this disease. Keratoconus is often associated eye allergies and excessive eye rubbing. It can start to affect vision in late teens and early 20’s and then cause progressive vision loss over years if not treated or maintained correctly.
Early signs of keratoconus can include:
- Mild blurring of vision
- Distortion
- Increased sensitivity to light and glare
- Eye redness
Late stage symptoms may include:
- Worsening blur not corrected with glasses or contact lenses
- Pathological increases in nearsightedness and astigmatism
- Unable to wear contact lenses
How is it diagnosed?
A comprehensive eye exam is needed to be done by your ophthalmologist, which can require a patient to go on sophisticated machines that map the surface curvature and topography of the cornea.
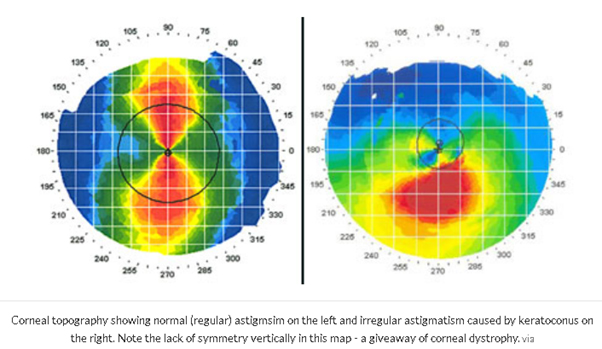
image source from https://www.eyedolatryblog.com/2017/05/keratoconus-is-much-more-prevalent-than.html
How is keratoconus managed?
Your ophthalmologist may recommend treatments based on the progression of keratoconus. Some options may include:
- Glasses
- Hard contact lenses
- Implantable contact lenses
- Collagen Cross linking
- Corneal transplant
It is very important that people with keratoconus to not rub their eyes. This can cause further thinning of the cornea.
Information and images sourced from the American Academy of Ophthalmology


 n
n